
by Jack Norris, RD
Contents
- Essential Information
- Additional Tips
- Iodine Sources
- Official Recommendations
- Iodine Antagonists
- Research on Iodine
- Iodine Deficiency
- Iodine Excess
- Measuring Iodine Status: Urinary Iodine Concentration
- Iodine Status of Vegans
- Appendix A: Studies Measuring Iodine Intakes via Food Tables
- Appendix B. Iodine Excretion while on a Lacto-Ovo-Vegetarian Diet
- Appendix C. Iodized Oil
- Bibliography
Essential Information
Iodine is important for a healthy thyroid. Iodine is found inconsistently in plant foods depending on the iodine content of the soil. The soil in many countries is low in iodine and so iodine has been added to some brands of table salt. You should make sure you have a source of iodine either from iodized salt or a supplement containing potassium iodide. For supplements, if convenient choose potassium iodide over kelp.
Additional Tips
When purchasing iodine, avoid stand-alone potassium iodide supplements that are intended to block radiation; they’re measured in milligrams (mg) rather than micrograms (abbreviated as µg or mcg) and can be many times the U.S. upper limit.
The United States upper limit for daily iodine intake is 1,100 µg. Although most adults can safely metabolize 1,100 µg, and even more, it’s prudent not to supplement beyond the United States recommended dietary allowance (RDA) for iodine which is 150 µg for adults.
If an iodine tablet contains significantly more iodine than what’s recommended, they can normally be broken into halves or quarters.
Iodine Sources
Iodine is consistently found in only a few foods: iodized salt, seaweeds, sea animals, and dairy products. Cows are given iodine supplements, and iodine in cleaning solutions are transferred to the milk.
In plant foods, iodine is found inconsistently depending on the iodine content of the soil; food grown near the ocean tends to be higher in iodine.
Plant milks fortified with iodine have an iodine content similar to cow’s milk but few are iodine-fortified (Bath, 2017; Vance, 2017). Unfortified commercial plant milks are very low in iodine (Ma, 2016; Bath, 2017).
Table Salt
In the United States, the voluntary addition of iodine to table salt was established in 1924 to prevent goiters which were prevalent at the time (Trumbo, 2016). Iodine-fortified table salt is required to be labeled as iodized and non-iodized table salt is required to be labeled with This salt does not supply iodide, a necessary nutrient (Office of the Federal Register).
Check the nutrition label for how much iodine is in a particular brand of iodized salt. The nutrition label might give a percentage of the Daily Value which is 150 µg, or it might give the amount in micrograms (µg), or both.
Although iodized salt can sometimes contain higher or lower amounts of iodine than advertised on the label (Dasgupta, 2008), salt iodization is viewed as one of the safest and most effective methods for achieving iodine sufficiency across a population and is not generally considered to be a source of excess iodine (Leung, 2014).
Salt in commercial and processed foods is usually not iodized (Dasgupta, 2008) and sea salt doesn’t contain appreciable amounts of iodine unless fortified.
Dasgupta et al. found that the iodine on the surface of salt may be lost to oxidation and that humidity can lead to some iodine loss from salt, so it’s best to keep the container sealed and, if you live in a humid environment, stored in the refrigerator.
Seaweeds
If someone regularly eats seaweed (multiple times a week), they’ll likely obtain adequate iodine; however, the availability of iodine from seaweed is variable and it can provide excessive amounts.
A survey of the iodine content of various seaweed products in the United Kingdom estimated an iodine content from zero to more than 10,000 µg per serving (Bouga, 2015); the upper limit set by the Institute of Medicine is 1,100 µg per day. For people with habitually high iodine intakes, typically from regular seaweed consumption, such large amounts of iodine probably won’t cause health problems; for people with habitually low iodine intakes, sporadic high iodine intakes might cause thyroid problems that are typically transitory (see our section Iodine Excess).
Nori, the seaweed used to wrap sushi rolls, is one exception. Studies of the iodine content of nori have found that six sushi rolls contain about 67 µg of iodine with a standard deviation of about 30 µg (see our spreadsheet on Sushi). This would suggest that people who eat sushi rolls on a daily basis will probably meet iodine needs without a supplement and without ingesting excessive amounts of iodine; because there are questions regarding the bioavailability of iodine from seaweeds, we can’t recommend nori as reliable source without studies measuring the iodine status of people who rely on it.
Kelp Supplements
In their 2019 review, Farebrother et al. say, “A survey of the U.S. prenatal multivitamins found significant discordance between label information and laboratory assay; 25 brands containing kelp contained between 33 and 610 µg per daily dose, the latter being almost three times the 220 µg recommended daily intake. This may be explained by the natural variations in kelp iodine content, and for this reason, kelp supplements should generally be avoided, and potassium iodide should be used in vitamin preparations.”
Most iodine supplements are simply tablets made from kelp. Being a seaweed, kelp likely contains at least small amounts of arsenic. There are some very rare cases in which people taking kelp supplements have developed symptoms of arsenic toxicity (Amster, 2007).
A survey of kelp supplements in the U.S. found that 8 out of 9 batches contained some level of arsenic (Amster, 2007), while a survey in the U.K. of imported seaweed found very little arsenic in kelp (Rose, 2007). In contrast, a 2017 ConsumerLabs.com report found arsenic contamination in only 1 of 6 supplements in the U.S., but they found excessive iodine in many of the supplements.
Official Recommendations
| Dietary Reference Intakes for Iodine | ||
|---|---|---|
| Age | US DRI (µg) |
Upper Limit (µg) |
| 0–6 mos | 110 | A |
| 7–12 mos | 130 | A |
| 1–3 | 90 | 200 |
| 4–8 | 90 | 300 |
| 9–13 | 120 | 600 |
| 14–18 | 150 | 900 |
| 19+ | 150 | 1,100 |
| Pregnancy | ||
| ≤18 | 220 | 900 |
| ≥18 | 220 | 1,100 |
| Breastfeeding | ||
| ≤18 | 290 | 900 |
| ≥18 | 290 | 1,100 |
| A. The Institute of Medicine says it’s not possible to establish an upper limit for 0–12 months old but that intake should be from food and formula only. | ||
Iodine Antagonists
Soy, flax seeds, and raw cruciferous vegetables (broccoli, Brussels sprouts, cauliflower, and cabbage) contain goitrogens that counteract iodine (NIH, 2020). In large amounts, or combined with iodine deficiency, goitrogens can exacerbate iodine deficiency or cause a goiter.
Theoretically, consuming large amounts of goitrogens could have a negative impact even when iodine intake is adequate, but this typically happens only in people who are exposed to unusually high amounts of goitrogens, such as those whose diets are largely based on cassava root (Chandra Amar, 2015).
Research on Iodine
In studies of vegans, their average urinary iodine concentrations tends to be lower than for other diet groups and for what is considered healthy. These lower iodine concentrations haven’t been correlated with thyroid problems among vegans; nonetheless, it’s prudent for vegans to meet iodine recommendations.
Zimmermann and Andersson report that in healthy adults the mean daily turnover of iodine is approximately 95 µg.
Ideally, we’d only recommend supplementing with enough iodine to make up for any difference between usual vegan intakes and the RDA, but there is very little data measuring iodine intakes from plant foods among vegans, which could vary considerably from country to country. Therefore, we recommend that vegans meet the RDA through supplements containing potassium iodide or through iodized table salt.
Iodine Deficiency
For centuries, iodine deficiency has been a problem in many regions due to a lack of iodine in the soil and food supply (Dasgupta, 2008). Too little iodine can result in hypothyroidism leading to an enlarged thyroid gland, known as a goiter.
Iodine deficiency among people who are pregnant or breastfeeding can inhibit brain development in the fetus and infant. In adults, hypothyroidism can lead to mental impairment, apathy, fatigue, weight gain, cold intolerance, constipation, and hair loss (British Thyroid Foundation, 2019; Linus Pauling Institute, 2015; National Institutes of Health, 2020). A systematic review found that subclinical hypothyroidism is associated with an increased risk of depression (RR 2.35, 95% CI 1.84 to 3.02; Loh, 2019).
Due to widespread deficiency, iodine fortification of table salt or bread has been implemented in many countries. In iodine-deficient regions that haven’t implemented fortification programs, the World Health Organization (p. 12, 2007) recommends supplementation for pregnant and lactating women (250 µg/day), women of reproductive age (150 µg/day), and children seven to 24 months of age (90 µg/day).
In regions that tend to be iodine replete, daily variations in iodine intake are unlikely to cause iodine deficiency; Andersen et al. (2008) report that “The thyroid gland has the capacity to store large amounts of iodine, unaffected by short-term low iodine intake.”
Iodine Excess
Excess iodine can result in hypothyroidism or hyperthyroidism. Often, the condition is due to iodine toxicity from medications or medical procedures, and is temporary; though in some cases it persists (Leung, 2014).
Hyperthyroidism from excess iodine can cause weight loss, tachycardia (high pulse rate), muscle weakness, skin warmth, and hair loss (British Thyroid Foundation, 2019; Linus Pauling Institute, 2015). There may be a connection between excess iodine and acne (Arbesman, 2005; Danby, 2007).
Bürgi (2010) says, “Most persons tolerate a chronic excess of 30 mg up to 2 g iodide per day, without clinical symptoms, but a detailed analysis reveals a persistent drop of serum T4 and T3 of 25% and 15%, respectively, and a rise of TSH of 2 mU/ l; all values, though, remain well within the normal range, and there are no clinical signs of thyroid dysfunction or goitre, even though sonographic thyroid volume is slightly increased.” Burgi considers iodine-induced hypothyroidism to be easily managed and says most cases are transient.
Dasgupta, et al. (2008) report that Japan has a high iodine intake ranging between 700 and 3,200 μg/d with excellent thyroid health, suggesting that excess iodine might be harmful only in areas where the population has adapted to low iodine intakes.
Farebrother, et al. (2019) report that high iodine intakes are a particular problem in populations with inadequate iodine that begin a supplementation program; intakes as low as 300 µg/day can trigger hyperthyroidism in individuals who are susceptible. They argue that the prevention of iodine deficiency through iodine fortification generally outweighs the risks of iodine excess, but monitoring should be conducted.
In a letter to the BMJ, Lewis (2016) argues that iodine excess does not cause autoimmune thyroid disease.
Measuring Iodine Status: Urinary Iodine Concentration
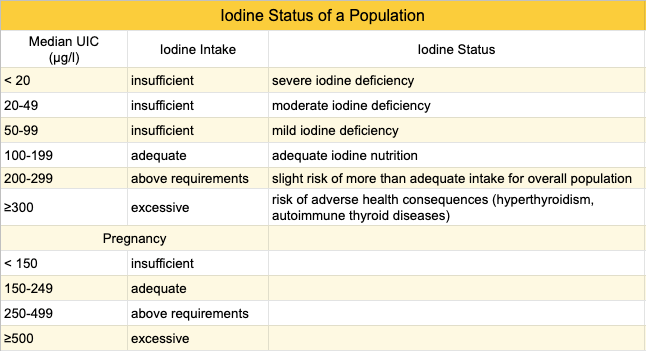
Average urinary iodine concentration (UIC) is used to determine the iodine status of a population. The World Health Organization (WHO) suggests these categories (WHO, 2007):
There are problems with using the WHO’s cutoffs to determine the iodine adequacy of an adult population: Iodine status has primarily been studied in school-age children and Zimmermann and Andersson (2012) point out that the WHO extrapolated adequate UIC levels for populations of school-age children to adults; they provide evidence that an adequate average UIC for an adult population is about 60 to 70 µg/l.
There’s also a large day-to-day variability in iodine intake and water consumption for any individual, with fasting and morning urine samples giving lower UIC values (Soldin, 2002). In order to compensate for the various issues with determining UIC, Andersen et al. recommend that 500 samples (not necessarily people) be used to determine a precise UIC for a population; though a sample size as low as 86 can estimate the UIC within a 10% margin of error (Andersen, 2008). For an individual, more than ten urine samples are recommended (Andersen, 2008).
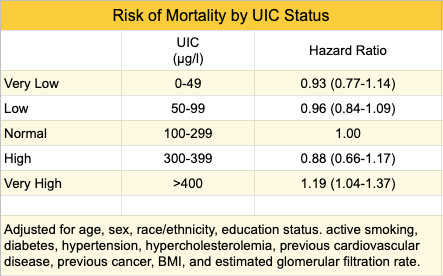
UIC and Mortality
A U.S. study estimated mortality rates according to urinary iodine concentration (UIC), utilizing a nationally representative sample of 12,264 adults, aged 20–80 years, enrolled in the National Health and Nutrition Examination Survey (NHANES) III from 1988 to 1994 (Inoue, 2018). The participants were followed for 19.2 years and the groups with very low and low UIC levels didn’t have an increased mortality rate while the group with a very high UIC level (>400) had a higher mortality rate. Although this study controlled for many confounding variables, it’s an observational study and the finding doesn’t necessarily indicate a causal relationship.
Iodine Status of Vegans
Research has raised concerns about the iodine status of vegans. In this section, we examine the research to assess how much concern is warranted.
UIC of Vegan Adults
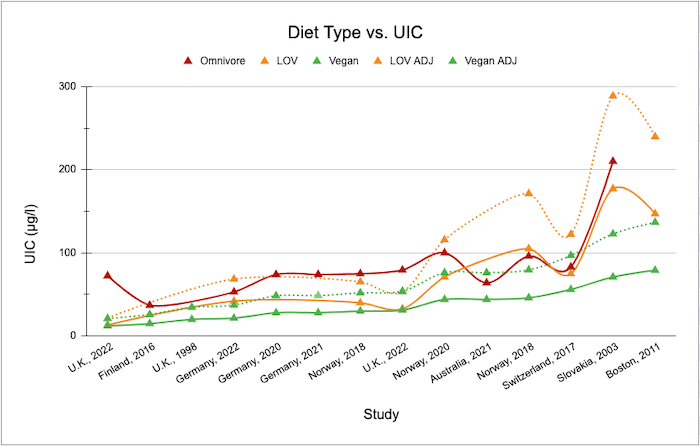
The chart below includes studies measuring the UIC of vegetarians and vegans. For our data presented below, a total of 501 vegans have been included in all studies with 710 samples taken. The most samples taken in an individual study is 212 (Schüpbach, 2017). The UIC sampling methods and the number of people included in studies on vegans are listed in the Summary tab of Iodine Supplementary Material for VeganHealth.
The typical UIC of vegans, depicted by the solid green line, is well below the 100 µg/l that the WHO recommends and only three of the 14 studies reach the 60 µg/l recommended by Zimmermann and Andersson. The dotted lines in the chart are explained in the next section, UIC and Urine Volume.
UIC and Urine Volume
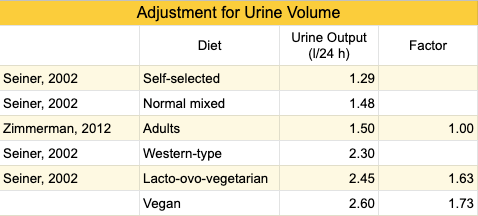
None of the studies measuring the UIC of vegans adjusted for urine volume, which could be higher for vegans due to plant foods containing more water, resulting in artificially low UIC measurements. One study has measured urine volume of people while on a lacto-ovo-vegetarian diet (Siener, 2002). In the table below, we used their data to adjust the UIC of lacto-ovo-vegetarians and vegans for urine volume. The dotted lines in the Diet Type vs. UIC figure (above) represent what the UIC for lacto-ovo-vegetarians and vegans might be if they were adjusted for urine volume, though this should be considered purely hypothetical.
Due to the higher average urine volume of vegans and lacto-ovo-vegetarians, we’ve added the dotted lines to the chart above, Diet Type vs. UIC, to show the UIC of vegans and lacto-ovo-vegetarians adjusted for urine volume. Once adjusted, six of the 14 studies on vegans show an average UIC above the 60 µg/l threshold recommended by Zimmermann and Andersson.
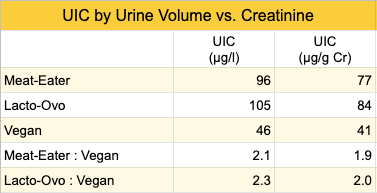
UIC and Creatinine
Soldin (2002) reports that urinary iodine to creatinine ratio (UI/Cr) is considered a more reliable measurement of iodine excretion than UIC measurements based on urine volume. Only one study of vegans included the UI/Cr ratio (Brantsaeter, 2018). The UIC ratio of meat-eaters and lacto-ovo-vegetarians to vegans is higher when based on urine volume than on creatinine (see table below), which provides more evidence that urine volume could be artificially lowering the UIC of vegans.
On the other hand, there’s evidence that meat-eaters have higher creatinine levels than vegetarians (Watt, 2004) and vegans (Lindqvist, 2020), which would at least somewhat counteract the effect of a higher volume of urine, making it complicated to assess the UIC of vegans using urine or creatinine.
Iodine Intake and UIC of Vegans
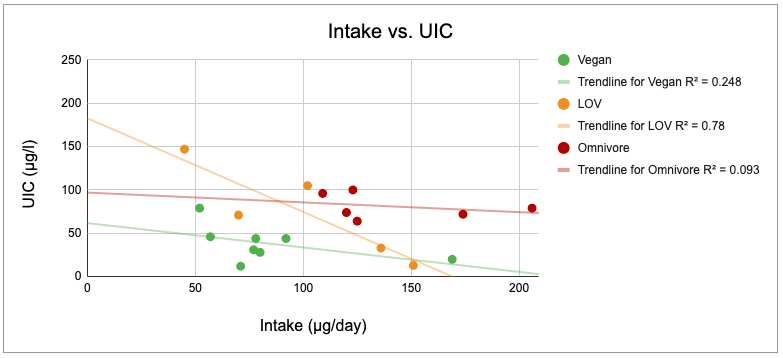
The chart below shows the relationship between iodine intake and UIC in studies of vegans. It’s odd that there appears to be an inverse association between iodine intake and UIC. This could be due to inaccurate assessment of iodine intake.
The study by Leung et al. (Boston, 2011) found that 24 of the 62 vegans were taking a multivitamin with iodine and two were taking either kelp or an iodine supplement; they had the highest average UIC (79 µg/l) measured among vegans which should give us confidence that iodine from multivitamins is an adequate source for vegans.
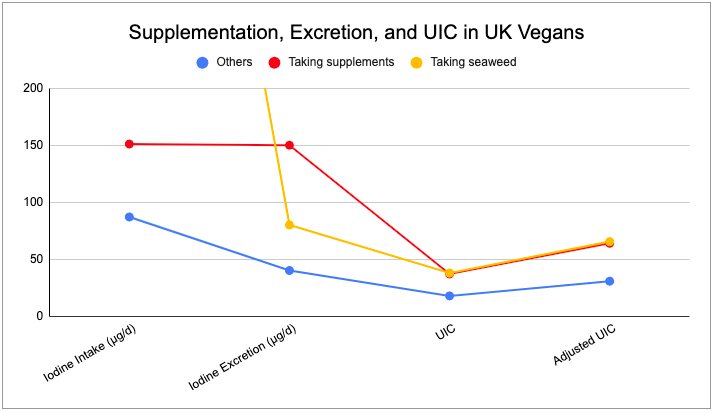
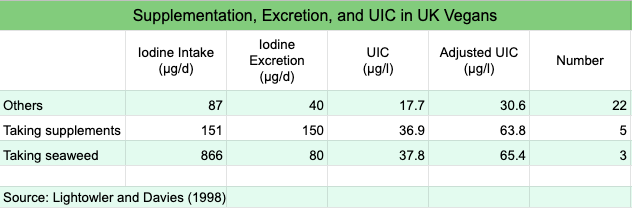
The study by Lightowler and Davies (1998) is worth a closer look. They used a a chemical analysis of duplicate portions of 4 days of food and urine to determine iodine intake and urinary iodine output of vegans in the U.K. They found that of the 30 vegans, 22 weren’t taking supplements or seaweed, 3 were taking seaweed, and 7 were taking supplements. The chart below shows their intakes and urinary iodine excretion. Iodine intakes for those eating seaweed were 866 µg/day. The results suggest that either the iodine in the seaweed wasn’t bioavailable, the intakes were misreported, or the iodine had cleared by the time the spot test was conducted.
Thyroid Hormone Levels of Vegans
With regard to the iodine status of individuals, Zimmermann and Andersson (2012) point out that UIC isn’t an appropriate indicator:
A common mistake is to assume that all subjects with a spot UIC <100 mg/L are iodine deficient. But dietary iodine intake and therefore UIC are highly variable from day to day. In iodine-sufficient countries where most iodine intake comes from iodized salt, UIC (both spot and 24-h urine collections) show an individual day-to-day variation of 30–40%.
Due to the limitations of assessing the iodine status of individuals based on UIC, we’ll turn our focus to the thyroid hormones.
Thyroid Stimulating Hormone Levels of Vegans
Less studied in vegans than UIC, but arguably more important, is thyroid-stimulating hormone (TSH). Although TSH is considered a poor indicator of iodine status, it’s a more direct indicator of thyroid health which is the objective of maintaining a healthy iodine status.
Normal TSH levels are typically considered to be between 0.5 to 5.0 mIU/l. In general, a higher TSH level is a sign of hypothyroidism in which more TSH is signaling the thyroid to produce the thyroid hormones T3 and T4. A lower TSH level is a sign of hyperthyroidism in which the body is not signaling the thyroid to produce more hormone because there’s already too much.
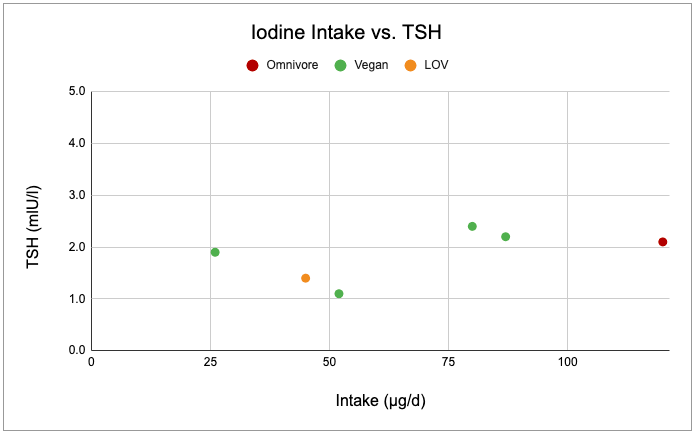
There are four studies reporting TSH levels in vegans (Key, 1992; Leung, 2011; Rauma, 1994; Weikert 2020). Except for a caveat regarding Key et al. (explained in the chart notes), the average TSH levels of the total of 150 vegans in these studies were, respectively, 2.2, 1.1, 2.1, and 2.4 mlU/l; all well within the normal range.
Using the best data we have and except when iodine intake is excessive, the chart below shows normal TSH levels for a range of usual iodine intakes among vegans.
Key et al. excluded three vegans from the average TSH measurement due to reporting taking kelp. These three vegans had very high TSH measurements of 11.3, 13.4, and 26.4 mlU/l and are excluded from the graph above of Iodine Intake vs. TSH. For these participants, there’s a small chance of reverse causality such that some were supplementing with iodine in response to a diagnosis of a high TSH. The remaining vegans in Key et al. reported taking no iodine supplements; two of these had elevated TSH levels of 5.3 and 8.3 mlU/l (and are included in the graph above).
Rauma et al. studied a small group of long-term, vegan raw foodists in Finland, many of whom had adopted the diet to treat medical conditions. Chemical analysis of duplicate food portions revealed an intake of 26 µg per day. All vegans had a TSH of under 4.0 except the vegan with the highest urinary iodine of 1,700 µg/day who had a TSH of 5.0 mlU/l (laboratory reference range was to 0.2–4.0 mlU/l).
One exception to the normal TSH levels among non-seaweed-eating vegans is reported in an obscure abstract (Crane, 1992) that I couldn’t locate, but that is described by Remer et al. The study was of vegans in the United States who used only non-iodized sea salt and had significantly reduced serum iodine concentrations; 25% had clearly elevated TSH levels and 12% had developed hypothyroidism.
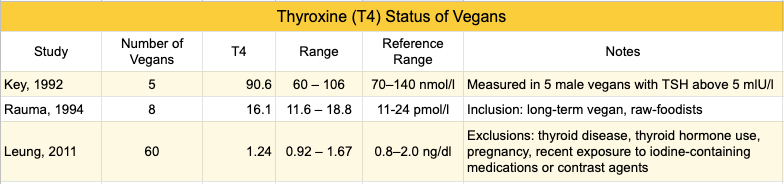
Thyroxine (T4) Levels of Vegans
The thyroid produces two hormones that regulate metabolism: triiodothyronine (T3) and thyroxine (T4). The thyroid mainly produces T4 (Farebrother, 2019). The half-life of T4 is 5 to 7 days, while the half-life of T3 is only 1 day (Medscape, 2016).
In the three studies measuring thyroid hormone levels of vegans, only one vegan had a T4 level below the reference range, and that was a participant in Key et al.’s study who was supplementing with seaweed (table below). Note that Leung et al. excluded participants who had thyroid disease, so only undiagnosed thyroid disease would have been detected in these subjects.
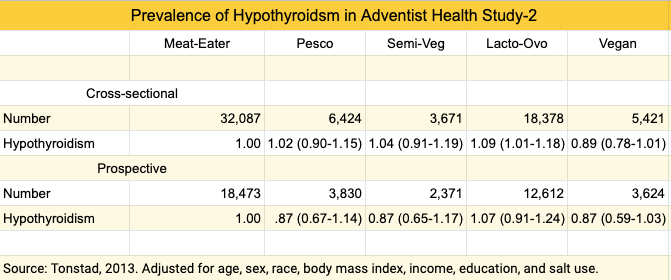
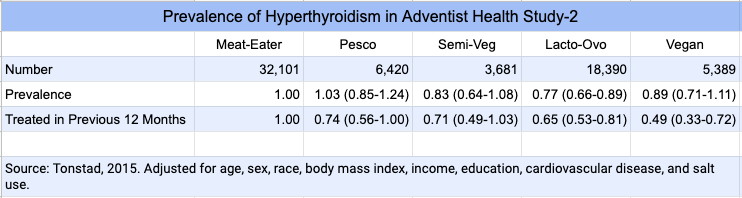
Thyroid Status in Adventist Health Study-2
The most direct way to determine the thyroid status of vegans is to measure their rates of thyroid disease. The data is limited, but we have reports from the Adventist Health Study-2 measuring the prevalence of hypothyroidism and hyperthyroidism.
The prevalence of hypothyroidism among Adventist Health Study-2 participants from the U.S. and Canada was reported both cross-sectionally and prospectively after about 4-6 years of follow-up (Tonstad, 2013). Lacto-ovo-vegetarians were more likely to have been treated for hypothyroidism in the previous year in the cross-sectional arm, while vegans had a trend towards less hypothyroidism in the prospective arm.
According to the authors, “While vegan diets are associated with lower body weight, which may protect against hypothyroidism, the lower risk among vegans existed even after controlling for [body mass index] and potential demographic confounders.” It’s not clear why lacto-ovo-vegetarians would have fared worse than meat-eaters. Adding salt to foods daily or more often than daily (compared to less than weekly) was associated with increased hypothyroidism among the entire population; this finding couldn’t be readily explained.
The Adventist Health Study-2 released a report measuring the prevalence of hyperthyroidism (Tonstad, 2015). Compared to meat-eaters, vegans had a similar prevalence of reporting having had hyperthyroidism in the previous year, though only half the prevalence of being treated for it.
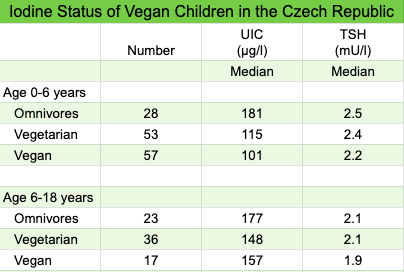
Iodine Status of Vegan Infants and Children
Světnička et al. (Czech Republic, 2023) compared the iodine status of omnivore, vegetarian, and vegan infants and children. The Czech Republic is considered iodine replete due to iodized table salt. The study found healthy iodine status in all groups, as seen in the table below.
Based on an iodine intake analysis, some of the children in all three diet groups appeared to be obtaining too little iodine, although iodized table salt wasn’t included in the analysis. The study also found a higher prevalence of positive titers of AhTGc among vegetarians and vegans which could indicate insufficient iodine intake or the beginnings of autoimmune thyroid disease. This finding should emphasize the importance of vegetarians and vegans obtaining a reliable source of iodine.
Iodine Content of Vegan Breastmilk
Pawlak et al. (2022, United States) compared the iodine content of breastmilk of 12 vegans, 6 vegetarians, and 12 omnivores; the median iodine content was 65 µg/L (32– 194 µg/L), 108 µg/L (62–189 µg/L), and 99 µg/L (62–1,719 µg/L) respectively. The difference between diet groups wasn’t statistically significant. Although 75% of the vegans used supplements, the researchers didn’t determine whether they contained iodine. The researchers estimated a daily iodine intake of each infant, assuming a daily breastmilk intake of 0.78 L per day, and found that 75% of vegans, 67% of vegetarians, and 58% of omnivores wouldn’t meet the DRI; the difference between diet groups wasn’t statistically significant. Markers of iodine deficiency among the infants weren’t measured. According to the researchers, the low iodine content of breastmilk could be more of a concern for vegan infants because vegan mothers are more likely to breastfeed and to breastfeed for longer periods than omnivores. The authors write that “[The American Thyroid Association] and the American Academy of Pediatrics (AAP) recommend using 150 µg/day iodine supplements during lactation. Only ~15% of lactating women in the United States adhere to this recommendation.”
Ureto-Valesco (Spain, 2023) found an average iodine intake of 260 µg among 20 vegetarian mothers (including 11 vegans) compared to 245 µg among 92 omnivore mothers. Amounts from supplements and iodized salt were included. 40% of vegetarians and 43% of omnivores had iodine intakes below the researchers’ recommendation of 209 µg/day. The average iodine content of breastmilk was 126.4 (SE 13.4) µg/L among vegetarians and 159.2 (SE 5.1) µg/L among omnivores.
Iodine Deficiency Cases among Vegan
Although many studies have shown lower iodine intakes, there have been few cases of frank iodine deficiency among vegans.
Yeliosof and Silverman (USA, 2018) reported a case of a vegan infant who developed iodine deficiency hypothyroidism between 19 and 23 months of age after being weaned off breastmilk. His mother had been using prenatal vitamins which provided iodine for her breastmilk but the infant wasn’t provided supplemental iodine after weaning.
Park et al. (United Kingdom, 2005) reported three cases of female vegans developing goiters, age 17, 21, and 36 years. The goiters were reduced through iodine supplementation with kelp being used in two of the patients.
Shaikh et al. (United Kingdom, 2003) reported a case of a vegan mother developing a goiter during pregnancy and who had an infant with a small goiter at 10 days old; both had elevated TSH. The mother’s usual iodine intake was estimated to be 43 µg/day. The goiter and thyroid hormones normalized in both patients after iodine supplementation.
Gordon et al. (United Kingdom, 2006) reported a case of a 15-year-old girl who developed a goiter and high TSH levels while on a diet that, while not completely vegan, excluded dairy and wheat (due to allergies) and also excluded red meat. Iodine treatment reduced her goiter size over 6 months.
Iodine Status of Vegans: Conclusion
Studies of vegans show them to have lower UIC than omnivores and typically well below the threshold of 100 µg/l that the WHO recommends for a population.
There are three potential problems with using UIC as a marker for the iodine status of adult vegans: 1) the WHO UIC threshold levels are likely too high for adult populations, 2) vegans may have a higher urine volume, and 3) studies of vegan don’t have the recommended number of samples needed to determine the UIC levels of a population. Taken together, UIC measurements have probably exaggerated estimates of iodine deficiency among vegans.
Direct markers of thyroid health, TSH and T4 levels, or a diagnosis of hypothyroidism or hyperthyroidism, tend to be normal in vegans, except in some cases of supplementation with seaweed or kelp supplements.
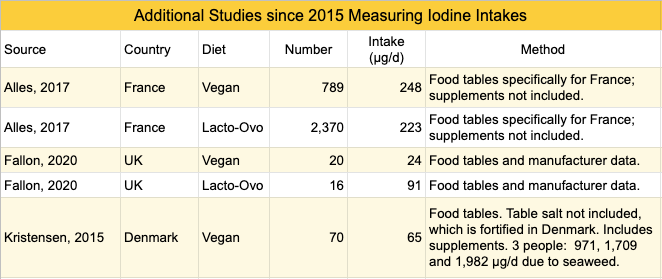
Appendix A: Studies Measuring Iodine Intakes via Food Tables
Although measuring iodine intakes via food tables is of questionable value due to high variability, for completeness this table lists the studies since 2015 that aren’t included in the above article.
Appendix B. Iodine Excretion while on a Lacto-Ovo-Vegetarian Diet
An experimental study in Germany placed 6 healthy adults on four separate diets for 5 days each, separated by a 9 day washout period (Remer, 1999). The diets were: 1) a normal omnivorous diet moderate in protein (ND), 2) a normal omnivorous diet high in protein (P), 3) a lacto-ovo-vegetarian diet (LOV), and 4) the ND diet again. They asked the participants not to use iodized table salt and to avoid iodine-rich foods in order to obtain a representative iodine content.
A chemical analysis revealed low amounts of iodine: 15.6 µg/day for the LOV and 35.2 µg/day for the ND. Urinary iodine output was 36.6 µg/day for the LOV compared to 50.2 µg/day for the ND.
The authors conclude that thyroid iodine losses must have contributed to the urinary iodine output and that a steady metabolic state had not been achieved. At the time, Germany was still experiencing endemic goiter with about 50% of the population having enlarged thyroid glands (Hampel, 1995). Subsequently, Germany initiated an iodized salt program (Khattak, 2016).
Appendix C. Iodized Oil
As an alternative to daily supplementation, the (World Health Organization (Table 2, p. 12, 2022) lists a single, yearly dose of 400 mg of iodized oil for during pregnancy and breastfeeding, and for women of reproductive age (400 mg), and a yearly dose of 200 mg for children up to two years old.
The World Health Organization doesn’t elaborate on iodized oil and we only found one relevant paper. Tonglet et al. (1992) conducted a study in a region of Zaire where iodine deficiency was common. They fed a single dose of iodized oil to people with goiters; this resulted in significantly correcting iodine deficiency for a year. Tonglet et al. concluded that the evidence was strong enough to warrant treating the entire population of the region with iodized oil. They noted that such treatment and its evaluation were in progress, but I couldn’t find any paper reporting on the follow-up nor any evidence that iodized oil is used to treat iodine deficiency today.
Bibliography
Last updated June 2023
Aakre I, Solli DD, Markhus MW, Mæhre HK, Dahl L, Henjum S, Alexander J, Korneliussen PA, Madsen L, Kjellevold M. Commercially available kelp and seaweed products – valuable iodine source or risk of excess intake? Food Nutr Res. 2021 Mar 30;65. Not cited. Measured iodine content of seaweed products in Norway.
Arbesman H. Dairy and acne–the iodine connection. J Am Acad Dermatol. 2005 Dec;53(6):1102.
British Thyroid Foundation. Hair loss and thyroid disorders. 2019. Accessed January 9, 2021.
Bürgi H. Iodine excess. Best Pract Res Clin Endocrinol Metab. 2010 Feb;24(1):107-15.
Chandra Amar K. Iodine, Thiocyanate and the Thyroid. Biochem Pharmacol (Los Angel) 2015;4:3. (PDF)
Chung HR. Iodine and thyroid function. Ann Pediatr Endocrinol Metab. 2014 Mar;19(1):8-12. Not cited.
Crane MG, Mullen T, Lukens R. Iodine status of total vegetarians. Second International Congress on Vegetarian Nutrition (Abstract) Arlington, Virginia, USA, 1992. Could not locate.
Danby FW. Acne and iodine: reply. J Am Acad Dermatol. 2007 Jan;56(1):164-5.
Draper A, Lewis J, Malhotra N, Wheeler E. The energy and nutrient intakes of different types of vegetarian: a case for supplements? Br J Nutr. 1993 Jan;69(1):3-19. Not cited. Provided nutrient intakes but superseded by more recent research.
Leung AM, Braverman LE. Consequences of excess iodine. Nat Rev Endocrinol. 2014 Mar;10(3):136-42.
Ma W, He X, Braverman L. Iodine content in milk alternatives. Thyroid. 2016 Sep;26(9):1308-10
Medscape. Irizarry L. Thyroid Hormone. Updated: Oct 12, 2016.
Pennington JA. A review of iodine toxicity reports. J Am Diet Assoc. 1990 Nov;90(11):1571-81. Not cited.
Soldin OP. Controversies in urinary iodine determinations. Clin Biochem. 2002 Nov;35(8):575-9.
6 thoughts on “Iodine”
One idea, Jack, might be to include a section “Possible symptoms of a(n) ___________ deficiency.”
A long-time vegan friend of mine was asking about iodine.
Hi George,
The deficiency symptoms are listed under Iodine Deficiency. But iodine deficiency symptoms aren’t easy to trace to iodine deficiency (other than a goiter which results from severe deficiency). Trying to diagnose one’s own iodine status isn’t reliable and vegans shouldn’t judge their iodine intake based on whether they have deficiency symptoms; rather they should make sure they have a reliable source. This is different than iron and zinc where I think it’s safer for vegans to assume that if they don’t have deficiency symptoms, the probability that they’re getting enough is high enough that they don’t need to worry about iron and zinc.
Hi,
Do algal oil supplements contribute significantly to iodine intake. I am wondering if I am taking a supplement containing 150mcg potassium iodide whether if I take a microalgae DHA supplement whether that would impact a lot on my total daily iodine intake.
Thank you for your time in reading this!
> Do algal oil supplements contribute significantly to iodine intake.
I’ve never seen that they do. I don’t know if companies test their products for iodine contamination or if they know that there’s no significant amount of iodine because of how it’s produced.
Is iodine needed for anything other than the thyroid? Is it still necessary to supplement iodine if one takes a levothyroxine supplement and thyroid levels are OK?
Iodine’s function in humans is as an essential component of the thyroid hormones. It would be best to discuss your situation with the provider who prescribed the levothyroxine,