
by Jack Norris, RD
Contents
- Essential Information
- Plant Food Sources of Calcium
- Official Recommendations
- Safety of Calcium Supplements
- Research on Calcium and Vegan Diets
- Bibliography
Essential Information
Vegan adults should eat 3 servings of good sources of calcium per day while teenagers should eat 4 servings. The image below shows good sources of calcium that are readily available in the United States. The image lists the amount of each food that qualifies as one serving.
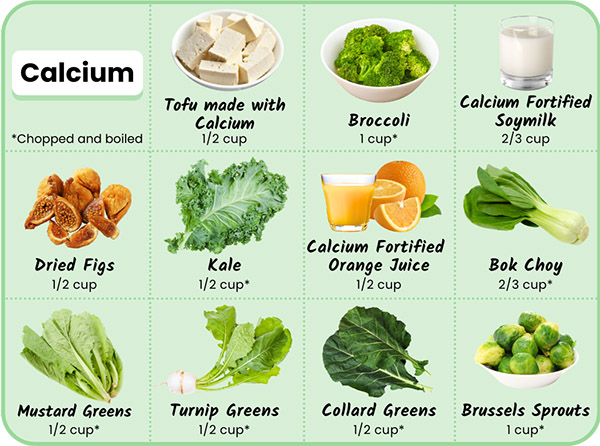
Luckily, most plant-based milks are fortified with calcium. And one of my favorite foods for obtaining calcium is tofu made with calcium salts, which is high in calcium and protein, both of which are good for bones. If you find it inconvenient to eat foods high in calcium each day, a calcium supplement of about 500 mg per day is another option.
Resistance exercise twice a week, involving lifting moderate weights, is possibly the most reliable way for people to increase the strength of their bones. We encourage everyone to follow such a program. Talk to your health professional about what program is right for you.
Plant Food Sources of Calcium
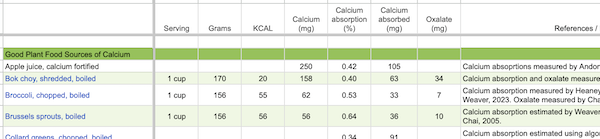
The spreadsheet Calcium and Oxalate Content of Plant Foods lists the amounts of calcium and absorption rates of various plant foods.
Most of the calcium amounts in that spreadsheet come from the USDA nutrient database, which lists an average of the samples they’ve analyzed. The amount of calcium in plant foods is somewhat dependent on the amount of calcium in the soil (Weaver, 2013).
The DRI for calcium is roughly based on an average absorption of calcium from foods of 25% (p. 38 in Dietary Reference Intakes, 2011). As a calcium dose increases, the percentage absorbed decreases. Beyond the size of the dose of calcium, the oxalate level in plant foods is the main determinant of how much calcium can be absorbed.
Official Recommendations
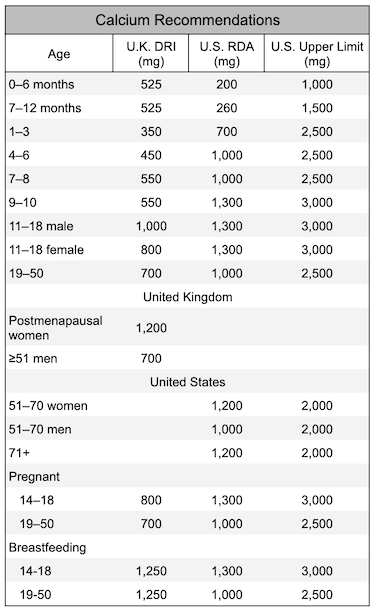
Below are the calcium intake recommendations for the United Kingdom and the United States. We recommend aiming to at least meet the U.K. recommendations. It’s safe to take a calcium supplement to make up the difference between your usual dietary intake and the recommendations.
The Daily Value for calcium on food labels is 1,300 mg.
Safety of Calcium Supplements
Summary: Calcium supplements of 1,000 mg per day appear to be safe among healthy people. People with chronic kidney disease should talk to their physicians about calcium supplements.
There are a variety of studies looking at the safety of calcium supplements with respect to heart disease, especially coronary artery calcification (CAC), and also colon cancer and kidney stones.
On behalf of the Calcium Supplements Treatment Trialists’ Collaboration, Huo et al. (2023) performed a meta-analysis of calcium supplement trials (1,000 to 1,500 mg per day). Their analysis included over 55,000 participants and was divided into 7 trials of calcium supplements alone and 6 trials of calcium and vitamin D supplements combined. They concluded that calcium supplements were not associated with any significant excess hazards for coronary heart disease and stroke outcomes, but included too few cases to rule out a (relatively small) increased risk of 0.3%–0.5% per year.
Wang, et al. (2010) studied the impact of calcium supplements on the risk of abdominal aortic calcification (AAC) and coronary artery calcification (CAC). Healthy postmenopausal women took part in a 5-year randomized trial; 718 received a placebo and 706 received 1,000 mg of calcium per day. Healthy middle-aged and older men took part in a 2-year randomized, placebo-controlled trial; 101 received a placebo, 101 received of 600 mg of calcium per day, and 96 received 1,200 mg of calcium per day. Neither dietary calcium nor calcium supplementation was related to changes in AAC or CAC.
The Framingham Study measured calcium intakes and followed participants for four years at which time they measured the amount of calcification of their arteries (Samelson, 2012). They found no correlation fkr calcification of the arteries with calcium intakes up to about 3,000 mg per day in either men or women or for calcium supplements of 500 mg per day or more compared to no supplements. Also see No Need to Worry About Calcium and Your Heart from the Tufts Health & Nutrition Letter (November, 2019).
The Multi-Ethnic Study of Atherosclerosis reported on the association between coronary artery calcification (CAC) and calcium intake (Anderson, 2016, United States). They followed participants free of CAC at baseline for 10 years. When not adjusting for calcium intake, supplement use was associated with a barely significant increased risk of CAC (RR: 1.12, 95% CI: 1.00-1.26, P=0.047). When the authors adjusted for calcium intake, calcium supplement use was associated with an increased risk of CAC (RR: 1.22, 95% CI: 1.07-1.39); this finding is hard to interpret because calcium intake influences both total calcium and calcium intake from supplements. Another perplexing aspect of this finding is that the people in the lowest calcium intake group, who only had an average calcium supplementation amount of 90.6 mg per day, had the highest risk of CAC. The authors state, “we did perform multiple testing, and it is possible that associations found may be attributed to chance.” Given that this is a prospective study, which is a weaker form of evidence than clinical trials, and that the findings of harm from calcium supplements were relatively weak or confounded, we don’t consider it as evidence to avoid calcium supplements. We’ve included a summary of this study because some nutritionists cite it to suggest calcium supplements should be avoided.
Colorectal cancer is another concern with regard to calcium supplements. As described in Calcium Supplements and Colorectal Cancer, one study found that long-term use of a 1,200 mg per day calcium supplement was associated with an increased risk of one type of polyp that can lead to colorectal cancer. This increased risk with higher calcium intakes was not seen in other studies although the other studies didn’t look at total calcium intake rather than supplements specifically. The authors of this study suggest that those with serrated polyps of the colon or rectum, especially women and smokers, avoid calcium supplements (Crockett 2018).
There’s been a concern that taking calcium supplements can increase the risk of kidney stones, but for the most part, research has shown that taking calcium supplements with meals can actually reduce the risk of calcium-oxalate kidney stones, the most common form of stone. For more information, see the article Oxalate.
Some studies have found an increased risk of kidney stones when taking both high-dose calcium and vitamin D supplements (Letavernier, 2018; Avenell, 2014). The amount of calcium taken in these studies tends to be 1,000 mg or higher (Lappe, 2017; Jackson, 2006).
Research on Calcium and Vegan Diets
There’s no reason to think that vegans are protected from osteoporosis more than other diet groups and they should strive to meet calcium recommendations.
The U.S. Recommended Dietary Allowance for calcium for adults is 1,000 to 1,200 mg per day depending on sex and age. The World Health Organization has similar recommendations (WHO, 2004). Although it’s possible to meet calcium recommendations by eating greens alone, the average vegan probably won’t meet recommendations without drinking a glass of a calcium-fortified beverage each day, eating calcium-set tofu, or taking a supplement.
Because vegans don’t eat dairy products, their calcium intakes tend to be low. Bickelmann et al. (2023) conducted a meta-analysis of observational studies measuring the calcium intakes of vegans, vegetarians, and meateaters. On average, vegans have a significantly lower intake of calcium, though in recent years the gap has closed (supplemental calcium included):
Before 2010:
- Vegans: 645 mg/d
- Vegetarians: 891 mg/d
- Meateaters: 866 to 955 mg/d
Since 2010:
- Vegans: 776 mg/d
- Vegetarians: 950 mg/d
- Meateaters: 918 to 1,017 mg/d
Animal Protein and Osteoporosis
As seen above, the calcium intake of vegans tends to be lower than lacto-ovo vegetarians, non-vegetarians, and the RDA. Traditionally, the vegan community has responded to this by saying osteoporosis is a disease of calcium loss from the bones, not a lack of calcium in the diet. This was based on two pieces of evidence.
The first piece is that ecological studies have shown that the countries with the highest intakes of dairy products (northern Europe and the USA) have higher rates of hip fractures than do Asian and African countries where much less milk is consumed. This can be explained by the second piece of evidence which is that studies show that after ingesting animal protein, people urinate large amounts of calcium. Therefore, the thinking goes, calcium intake isn’t important for preventing osteoporosis and vegans are protected due to the lack of animal protein in their diets.
Let’s examine this evidence.
Observational Studies
While it’s true that Asian countries have lower rates of hip fractures than do higher dairy-consuming countries, it turns out that hip fracture rates can be misleading. The first prospective cohort study measuring clinically diagnosed vertebral fractures in an Asian population, the Hong Kong Osteoporosis Study, found that while hip fracture rates were lower in Hong Kong than Sweden, vertebral fracture rates were higher (Bow, 2012), as shown in the image below.
Bow et al. state:
The observed ethnic differences in fracture incidences may be due to the fact that hip fracture risk was affected by fall risk, whereas the risk of vertebral fracture mostly depends on bone strength. Despite the low hip fracture rate in our population, Hong Kong women had a higher prevalence of osteoporosis than US Caucasian women (35.8% vs. 20%, respectively) and a similar prevalence of about 6% in Hong Kong and US Caucasian men.
In other words, at least in this group of people from Hong Kong, the Chinese don’t have lower rates of osteoporosis.
Darling et al. (2009) conducted a systematic review and meta-analysis of 28 studies on protein and bone health including cross-sectional, prospective cohort, and intervention trials. Overall, there was very little evidence of a negative influence of protein intake on bone mineral density (BMD) with most cohort studies reporting either no influence or a positive influence. One study reported a significant increase in risk with increasing animal protein intake and increasing animal to vegetable protein ratio. Three studies found a decreased relative risk of hip fracture with increasing animal, total, and vegetable protein intakes. Two studies found no significant association of animal protein with fracture risk, whereas 2 studies found no association of total protein intake with fracture risk. The authors declared no conflict of interest.
Shams-White, et al. (2017) conducted a meta-analysis of 20 prospective observational studies and 16 randomized controlled trials and found no significant association between dietary protein and fracture risk. There was some evidence that more protein reduced bone loss of the lumbar spine among older adults. The study was supported by the Egg Nutrition Center and Dairy Management Inc. who were said not to have had any role in the design, analysis, interpretation, or presentation of the data or the results.
In a study from France (included in the meta-analysis by Shams-White et al.), Dargent-Molina, 2008 found that among women with calcium intakes lower than 400 mg/day, protein intake, which they suggested was mostly animal protein, increased the risk of fracture. In a study from Sweden, Michaëlsson 2014 et al. (2014) found that milk consumption was positively associated with early death in both men and women, as well as fractures, especially hip fractures, in women. While statistically significant, differences weren’t large enough to indicate dairy plays more than a small role in early death or fractures.
Metabolic Studies
As mentioned above, there is a theory that protein increases osteoporosis by increasing a loss of calcium through the urine. The idea is that protein, especially through the sulfur-containing amino acids, increases the acid in the blood which, in turn, gets shuttled to the urine, increasing the renal acid load. In order to neutralize that acid, calcium is used as a buffer and then urinated out with the acid.
There has been an enormous amount of research on protein and bone health and this view of protein causing osteoporosis has been refuted. Here are some of the main points of a 2012 literature review (Calvez, 2012) of clinical trials on the subject:
- Many clinical trials show that adding purified proteins to the diet increases calcium excretion through the urine. But when whole foods are eaten, this effect is not strong. And phosphorus, in which meat and dairy are rich, counteracts the increase of calcium in the urine between 40 and 65%.
- High protein diets increase acid excretion in the urine, but this can be handled by the body’s acid buffer system without the need for calcium.
- In low-calcium, but not high-calcium diets, higher protein intakes probably increase calcium absorption from the digestive tract causing an increase in calcium excretion in the urine.
- Fruits and vegetables are beneficial to bone health, probably due to their high potassium and magnesium content. This could cause confounding in protein studies because diets high in protein are often low in fruits and vegetables.
- There is some evidence that a beneficial effect of protein on bones is only seen when calcium intake and vitamin D status is adequate.
- Maintenance of adequate bone strength and density with aging is dependent on adequate muscle mass which is dependent on adequate intake of protein.
- An increase in IGF-1 is most likely the mechanism for increased bone health with higher protein intakes.
They conclude:
Although HP [high protein] diets induce an increase in net acid and urinary calcium excretion, they do not seem to be linked to impaired calcium balance and no clinical data support the hypothesis of a detrimental effect of HP diet on bone health, except in the context of inadequate calcium supply.
Another 2009 meta-analysis found that among five well-designed studies measuring calcium balance, net acid excretion was not associated with either decreased calcium balance or a marker of bone deterioration (Fenton, 2009).
Causes of Osteoporosis?
If animal protein doesn’t cause osteoporosis, what does?
Genetics likely play a strong role in osteoporosis, and, possibly related, estrogen levels in women. Among factors that can be controlled by lifestyle and diet, there has been evidence for the following:
Helps prevent:
- Weight-bearing exercise throughout one’s lifetime
- Higher body weight
- Adequate intake of calcium, vitamin D, vitamin K, phosphorus, potassium, magnesium, and boron
Contributes to:
- High sodium and caffeine intake
- Smoking
- Too little protein
- Excessive vitamin A (retinol, not beta-carotene)
- Possibly vitamin B12 deficiency
Calcium and Vitamin D
Some background: When calcium levels in the blood drop, parathyroid hormone (PTH) is released. PTH causes calcium to be released from the bones, thus raising the low calcium levels in the blood. Osteoporosis may result from chronically high levels of PTH. The conversion of 25-hydroxyvitamin D to calcitriol is also somewhat regulated by PTH levels (Groff, 2000). Calcitriol increases absorption of calcium and phosphorus (another major component of bones) from the intestines and decreases their excretion in the urine. In so doing, calcium levels in the blood rise and PTH levels drop.
Research has shown that, on average, Americans are getting enough calcium. Bischoff-Ferrari, et al. (2007) conducted a meta-analysis of prospective studies and randomized controlled trials and found that calcium intake and calcium supplements were not associated with a lower risk for hip fractures. Bolland, et al. (2015) conducted a meta-analysis of 44 cohort studies and found that dietary calcium between about 800 to 1,000 mg per day isn’t associated with risk of fracture, and there’s no evidence that increasing dietary calcium within that range or higher prevents fractures. An exception is that calcium and vitamin D supplements have been found to help women aged 69 to 106 years old who normally have low calcium intake and poor vitamin D status.
Vitamin B12 and Bone Mineral Density
Taking vitamin B12 might also be important for bone mineral density.
Low vitamin B12 status can result in elevated homocysteine which might harm bones. A cross-sectional study from Slovakia compared lacto-ovo-vegetarian women to omnivores (Krivosikova, 2009). The vegetarians had lower B12 levels (246 vs. 302 pmol/l) and higher homocysteine levels (16.5 vs. 12.5 µmol/l). In the four bone locations examined, vegetarians had lower bone mineral density than omnivores in two locations, and their higher homocysteine levels were negatively associated with bone mineral density in three locations. The bone mineral density associations appeared not to be adjusted for body mass index which, while not statistically different between the vegetarians and omnivores (23.9 vs. 25.0, respectively), is an important factor impacting bone mineral density.
A cross-sectional study from Germany found that male vegans and lacto-ovo-vegetarians had similar markers of bone turnover to each other, but higher markers than male omnivores (Herrmann, 2009). The vegans had a rather high average methylmalonic acid level of 727 nmol/l, indicative of significant vitamin B12 deficiency. None of the participants were taking B12, calcium, or vitamin D supplements. Upon stratifying the subjects into two groups based on their B12 status, the group with poor B12 status had higher markers of bone turnover. However, since almost all the people in the poor B12 status group were vegan or vegetarian (62 out of 63), and few vegans or vegetarians were in the replete B12 group (6 out of 66), it’s not clear that the increased bone turnover markers were due to poor B12 status or some other factor common to vegans and vegetarians.
Selenium and Bone Mineral Density
In a prospective study from the U.K. of 1,144 post-menopausal women with normal thyroid function, higher selenium levels were associated with greater bone mineral density (Hoag, 2012). Although selenium metabolism is involved in thyroid function, the study found that the associations between selenium and bone mineral density were independent of thyroid function. After 6 years of follow-up, selenium levels were not associated with bone fractures. Because selenium intakes can be low in vegan diets in some countries, it’s important that vegans in those countries ensure an adequate source (see Selenium).
Research on Vegans
Bone Mineral Density
A number of small, cross-sectional studies have shown vegans to have the same or slightly lower bone mineral density as non-vegans (Barr, 1998; Lau, 1998; Parsons, 1997; Ho-Pham, 2009a).
Ho-Pham, et al. (2009b) conducted a meta-analysis looking at the bone mineral density of vegetarians, concluding that “[T]here is a modest effect of vegetarian diets, particularly a vegan diet, on [bone mineral density], but the effect size is unlikely to result in a clinically important increase in fracture risk.”
A Denmark study found that vegans (n=78) had higher levels of parathyroid hormone (PTH) and bone-specific alkaline phosphatase (BAP) than omnivores (n=78) (Hansen, 2018). Vegan PTH was within the normal range while BAP might have been slightly elevated for a small number of vegans. It’s not clear if these markers were of clinical significance.
Quantitative Ultrasound
Quantitative ultrasound (QUS) is a method for indirectly measuring bone mineral density.
Menzel et al. (Germany, 2021) performed an interesting cross-sectional study of the differences in bone and nutrition status between 36 vegans and 36 omnivores; each group was 50% female.
They measured bone status using quantitative ultrasound of the calcaneus bone. They analyzed the data using reduced rank regression (RRR) in which they mixed vegans and omnivores together to see if some of the associations they found between nutrient status and bone health in vegans were also found in the omnivores (suggesting more strongly that they might be causal among vegans).
The nutrition factors most associated with bone health, in order of importance, were: plasma lysine, urinary iodine, thyroid-stimulating hormone (TSH), plasma selenoprotein P, plasma vitamin A, plasma leucine, plasma n-3 fatty acids, urinary calcium and magnesium, and plasma vitamin B6. We examine many of these factors in more detail in the article Bone Fractures among U.K. Vegans: Implications and Recommendations.
UK Biobank (2023)
In a large prospective British cohort of almost 500,000 men and women, vegetarians were at a higher risk of hip fracture compared to regular meat-eaters (HR 1.50, 95% CI: 1.18-1.91), the equivalent of an adjusted absolute risk difference of 3.2 (95% CI: 1.2-5.8) more hip fractures per 1,000 people over a 10 year period (Webster, 2023). The researchers described this difference in absolute risk as “modest.”
In an analysis separating the vegans from lacto-ovo-vegetarians, there were only 10 cases of hip fractures among vegans but that was enough to reach a statistically significant difference as compared to regular meat-eaters (HR 3.26, 95% CI: 1.75-6.08).
Differences between the body mass index of the vegetarians (25.6) and meat-eaters (27.3) could only explain 28% of the difference in hip fracture risk. Nutrient intake wasn’t assessed.
Adventist Health Study-2 (2021 & 2014)
Thorpe et al. (2021) published a report from the Adventist Health Study-2 comparing hip fracture rates of different diet groups among white participants only (due to their generally poorer bone health) who were 45 years or older.
Female vegans had a higher risk of hip fracture compared to non-vegetarians (HR 1.55, CI 1.06-2.26). These findings were adjusted for weight and height, but not for body mass index (BMI), so it’s hard to know if the difference is mainly due to the lower BMI of vegans which has been found in the Adventist Health Study-2 (see Cardiovascular Disease Markers of Vegans: 2013 Report from Adventist Health Study-2).
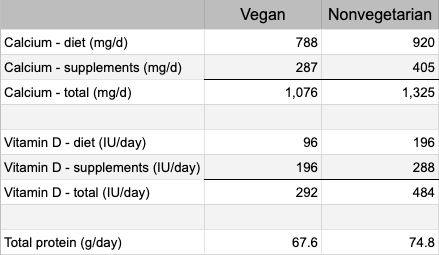
The findings were also adjusted for total calcium intake and total vitamin D intake, but not for protein intake. The table below shows the intakes of vegans and nonvegetarians.
After adjusting for calcium and vitamin D supplementation together, the researchers found that the vegans no longer had a higher risk of hip fracture. Their conclusion was that without supplementation of both vitamin D and calcium, female vegans are at high risk of hip fracture.
A previous report from Adventist Health Study-2 (AHS-2) examined caucasian Seventh-day Adventists living in the USA, comparing the intakes of many different foods and hip fracture risk after 5 years of follow-up (Lousuebsakul-Matthews, 2014). The study found that eating meat alternatives once a day or more (compared to less than once per week) was associated with a 66% reduced risk of hip fracture in the vegetarians (0.34, 0.12-0.95). Eating legumes once per day or more (compared to less than once per week) was associated with a 55% reduced risk in vegetarians (0.45, 0.22-0.94).
EPIC-Oxford (2020 & 2007)
A report from EPIC-Oxford (Tong, 2020) found a higher rate of bone fracture among vegans without any obvious explanation. Although vegans had a lower average calcium intake (591 mg/day compared to ~1,000 mg/day for other diet groups), there was little association between calcium intakes and a higher risk of fracture. See Bone Fractures among U.K. Vegans: Implications and Recommendations for more information.
A previous analysis from EPIC-Oxford (Appleby, 2007) found vegans to have a 30% higher fracture rate than meat-eaters (RR 1.30, CI 1.02-1.66) after adjusting for smoking, alcohol, body mass index, walking, cycling, vigorous exercise, other exercise, physical activity at work, marital status, parity and hormone replacement therapy. When the results were adjusted for calcium intake, the vegans no longer had a higher fracture rate. Among the subjects whose diets contained ≥525 mg of calcium a day (only 55% of the vegans compared to about 95% of the other diet groups), vegans had the same fracture rates as the other diet groups.
The authors of the UK Biobank study point out a limitation of this report from Adventist Health Study-2 which is that hip fractures were identified from self-reported questionnaires prone to selective loss to follow-up as compared to hospital records used in the UK cohorts described above (Webster, 2023).
Buddhist Nuns (Vietnam, 2011)
Ho-Pham et al. (2011) studied 88 vegans and 93 omnivores. After two years of follow-up, 5 vegans and 5 omnivores had sustained a new vertebral fracture; there was no significant difference between the two groups.
Food questionnaires indicated that the vegans were only eating an average of 1,093 calories, 36 g of protein, and 360 mg of calcium per day. The estimated energy requirement for women their age and size is about 1,600 calories indicating possible underestimation. The non-vegan nuns had intakes of 1,429 calories, 62 g of protein, and 590 mg of calcium per day which seems more plausible.
Ten fractures in 181 women in two years is high. The rate of vertebral fracture in women over 65 in Hong Kong and Japan is 594/100,000 person-years (Ho-Pham, 2009a). The fracture rate in this Buddhist nun study works out to be 2,762/100,000 person-years. The fractures in the Buddhist nun study were determined by x-raying each subject, rather than reporting a bone break, and would likely find more fractures than the study determining the 594/100,000 rate.
In summary, compared to non-vegetarian Buddhist nuns, vegan nuns had a similar rate of vertebral fractures, but it appears that the rates for both groups were high.
Bibliography
Groff J, Gropper S. Advanced Nutrition and Human Metabolism, 3rd ed. Wadsworth: 2000.
Ho-Pham 2009a. Ho-Pham LT, Nguyen PL, Le TT, Doan TA, Tran NT, Le TA, Nguyen TV. Veganism, bone mineral density, and body composition: a study in Buddhist nuns. Osteoporos Int. 2009 Apr 7. (Epub ahead of print)
Ho-Pham 2009b. Ho-Pham LT, Nguyen ND, Nguyen TV. Effect of vegetarian diets on bone mineral density: a Bayesian meta-analysis. Am J Clin Nutr. 2009 Oct;90(4):943-50.
Wang TK, Bolland MJ, van Pelt NC, Horne AM, Mason BH, Ames RW, Grey AB, Ruygrok PN, Gamble GD, Reid IR. Relationships between vascular calcification, calcium metabolism, bone density, and fractures. J Bone Miner Res. 2010 Dec;25(12):2777-85. Erratum in: J Bone Miner Res. 2011 Feb;26(2):439. The erratum listed for this abstract appears to itself be an erratum as it doesn’t apply to this paper.
Weaver 2013. Correspondence from Connie M. Weaver, PhD, Purdue University, Nutrition Science. September 2013.
26 thoughts on “Calcium”
hi, i’m a new vegan but if i scan the barcode of fortified plant milks with the Yuka app, it gives a warning about calcium carbonate (with more detail if you then click on “learn more”); it explains that calcium carbonate contains calcium nanoparticles that can penetrate biological barriers (so i assume they can also cross the bbb or blood-brain barrier) and therefore accumulate at cellular levels and we don’t know the long term effects of this. what do you think? are you familiar with this issue? it concerns me. on paper, it is the only downside of a well-planned vegan diet that i know of.
Francis,
I’d never heard of calcium carbonate nanoparticles until now. I did a quick search using AI and found this:
hi! I’ve got a question about something I would like to confirm with you because I’m not sure i understood you or not. If for instance the recommended amount of calcium is 500mg (WHO), does it mean we need 500mg of bioavailable calcium or 500mg of calcium no matter its absorbability?
Suzy,
The WHO’s calcium recommendations are basically the same as the United States DRI, which is 1,000 mg from adults 19 to 50 years old. The DRIs assume an absorption rate from foods of 25%. So, to answer your question, the recommendations are for total calcium rather than bioavailable calcium and they assume that people are getting an average amount of absorbable calcium.
Hello Jack. I like very much this blog, first of all. I usually eat 2 tablespoons of sesame seeds, previously roasted for 5/7 minutes at low temperature and then ground. Is it a good source of calcium, regarding its absorption ? As you know, these seeds are famous for its high level of this mineral.
Martin,
I don’t know what rate calcium is absorbed from sesame seeds. I haven’t seen any research on it.
Hi. I’ve found information about bioavailability of calcium from food. Sesame seeds included (~20% absorption rate).
https://doi.org/10.1080/10408398.2022.2107997
TZ,
Koeder and Perez-Cueto cite Weaver and Plawecki (1994) who compare the difference between calcium absorption from sesame seeds and nonfat dry milk in rats to humans. Since it’s not a direct measurement of calcium absorption in humans, I don’t consider it reliable.
Hey, as someone who lives in a country that makes it hard to find mostly of the greens here that have low oxalate besides broccoli and with prices of plant milks ridiculously high, do you think taking supplementation from calcium carbonate powder (the only vegan friendly source as other sources are calcium + animal derived vitamin D) should be warranted?
Simon,
Yes, calcium carbonate powder seems like a valuable way to meet a vegan’s calcium needs under such circumstances.
Correction: Under Calcium tips, the daily value should be 1,300 mg.
Thank you. It went from 1,000 to 1,300 in 2021. I’ve updated the article.
If someone chooses to take a calcium supplement, do you believe that the form of the supplement matters? This study from 1987 says that there is not much difference in the rate of absorption between different forms. Personally, as a person who is prone to getting migraines, I have found that I need to avoid calcium citrate, because the large amount of citric acid can contribute to a headache for me, which is an unusual reaction but it might be of interest to a few people who have the same problem. Interestingly, I can take zinc citrate because the dose is so much smaller.
https://pubmed.ncbi.nlm.nih.gov/3614304/
I haven’t seen enough evidence to conclude that one form is better than another.
Just an FYI. Noticed it wasn’t in the references. https://www.ncbi.nlm.nih.gov/pubmed/30376075
Thanks. We reviewed the article and listed it under “also reviewed” below the references.
Are fortified foods more regulated in the US & other countries & will actually contain the doses stated compared to supplements which sometimes don’t contain what they claim?
Regarding plant milks: Is this a cause for concern? (should we be writing to Oatly & the like..?) https://www.ncbi.nlm.nih.gov/pubmed/31791225
Thanks!
We looked into this and added a blog post about it here: https://veganhealth.org/study-examines-emerging-mycotoxins-in-plant-milks/
We don’t have any studies showing that humans consuming any levels of these emerging mycotoxins experience any sort of harm. Based on this evidence, we don’t see a need to advise the avoidance of plant milks.
It seems pretty clear from the research that vegans who get enough calcium do not have a higher risk of osteoporosis than the general population. But what about someone with osteoporosis (who is not taking drugs for it) who begins a vegan diet? Is there an increased risk of worsening osteoporosis, even with sufficient calcium and vit D in the diet? I have been unable to find research that addresses this population.
Thanks.
We are unaware of any research on vegans with osteoporosis.
I am currently pregnant and following a WFPB vegan diet. My OB/GYN suggested that I take a 500mg calcium supplement every day in addition to my prenatal vitamin, which does not contain calcium. But the only calcium supplements I can find also have vitamin D in them, and my prenatal vitamin already has 1000 IU of vitamin D, so I don’t want to get too much vitamin D. Also, many in the WFPB community recommend getting calcium from food rather than from supplements due to the risk of heart disease. But I’m concerned that I won’t get enough calcium from my diet alone, though I’m trying to eat kale, broccoli, and fortified orange juice every day. So I’m very confused now, and I’m not sure what to do. What would you recommend? Thank you!
The Recommended Dietary Allowance for pregnancy is 1000 milligrams per day. This calcium is used to maintain your bones and teeth and to support the development of your baby’s bones and teeth. You can see how much calcium is in some plant foods here. Calcium-fortified orange juice has around 350 milligrams in an 8-ounce glass. Try adding up the calcium you are getting from your diet for a few days to see if a supplement is needed (if you’re usually below 1000 mg). There are calcium supplements that don’t contain vitamin D but if you can’t find one, see how much vitamin D you’d be getting from the prenatal supplement + the calcium supplement + any vitamin D in the orange juice. You want to stay below 4000 IU of vitamin D a day.
As far as the concern with calcium supplements and heart disease, see Vegan Health’s article on calcium supplements – a 500 mg supplement does not seem to be a problem.
Is the calcium in roasted or sauteed dark green vegetables absorbed as well as boiled?
The calcium in dark green vegetables that are high in oxalates (like spinach and Swiss chard) is likely to be better absorbed from boiled vegetables than from roasted or sauteed vegetables. There is some evidence that boiling these vegetables and discarding the cooking water decreases the vegetables’ oxalate content. Theoretically this would reduce the likelihood that the vegetables’ oxalates would bind with calcium from the vegetables in the intestinal tract and prevent absorption of the calcium.
I could not find evidence for the effect of different types of cooking on calcium absorption from dark green vegetables that are not high in oxalates although I suspect that there would be little or no effect of cooking method.
Awesome, thanks for looking into this & duckweed ! Any idea about the levels stated in supplements vs in fortified foods which actually contain the doses stated/have more controls & regulations? Thanks!
The U.S. Food and Drug Administration does not require proof of nutrient content for fortified foods and supplements before they go to market – in other words, manufacturers report the nutrient content and that is goes on the Nutrition Facts label. The only way to know the nutrient content for sure is to pull an item off the shelf and have a lab test it.